Untreatable ‘super gonorrhea’ on the rise, spread by oral sex: World Health Organization.
The World Health Organization is sending a warning to the public.
A person can get gonorrhoea in their genitals, rectum and throat, but the last category is the one that is most concerning doctors.
A new mutant “super gonorrhea” is spreading through oral sex! And it’s not treatable with the current medicine.
Gonorrhea is the second most commonly reported STD in the U.S.
78 millon people get Gonorrhea every year.
It’s usually treatable with antibiotics. However there are new strains of the STD that are not responding to normal treatments.
Gonorrhea spreads through intercourse, oral and anal sex.
It generally infects warm, moist areas of the body.
Because symptoms of oral Gonorrhea are similar to other throat infections such as strep, doctors will often prescribe the wrong antibiotics.
The drugs kill some Gonorrhea bacteria but antibiotic-resistant ones remain in the back of your throat and spread through oral sex.
Experts think it mostly spreads during blowjobs where the genitals tough the pharynx A.K.A the very back of your throat.
“the bacteria that cause Gonorrhea are particularly smart.” Dr. Teodora Wi at W.H.O.
Experts say the best prevention is using condoms during any and all type of sex.
And getting tested often.
From CDC
Antibiotic resistance (AR) is the ability of bacteria to resist the effects of the drugs used to treat them. This means the germs are not killed and they will continue to reproduce.
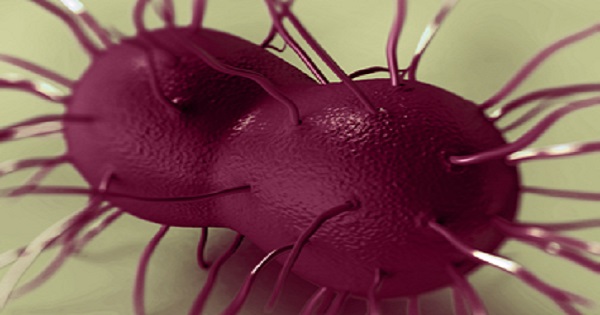
Neisseria (N.) gonorrhoeae, the bacteria that cause the STD gonorrhea, has developed resistance to nearly all of the antibiotics used for gonorrhea treatment: sulfonilamides, penicillin, tetracycline, and fluoroquinolones, such as ciprofloxacin.
We are currently down to one last effective class of antibiotics, cephalosporins, to treat this common infection. This is an urgent public health threat because gonorrhea control in the United States largely relies on effective antibiotic therapy.
Given the bacteria’s ability to adapt and survive antibiotics, it is critical to continuously monitor for antibiotic resistance and encourage research and development of new treatment regimens for gonorrhea.
Surveillance for antimicrobial resistance in N. gonorrhoeae in the United States is conducted through the Gonococcal Isolate Surveillance Project (GISP).
Each year, 25–30 sites and 4–5 regional laboratories across the United States participate in GISP and collect thousands of N. gonorrhoeae samples from men with urethral gonorrhea at STD clinics. Isolates from these samples are then used by researchers to determine the bacteria’s susceptibility to a given set of antibiotics.
Since 1989, data from this project have directly contributed to updating CDC’s STD Treatment Guidelines for gonorrhea.
Clinicians are asked to report any N. gonorrhoeae specimen with decreased cephalosporin susceptibility and any gonorrhea cephalosporin treatment failure to CDC through their state or local public health authority.
Bacteria have decreased susceptibility to a given antibiotic when laboratory results indicate that higher-than-expected antibiotic concentrations are needed to stop their growth.
In the United States, reports of apparent failures of infections to respond to treatment with CDC-recommended therapies should be reported to Robert D. Kirkcaldy, MD, MPH ([email protected]; 404-639-8659), Surveillance & Data Management Branch, Division of STD Prevention, Centers for Disease Control and Prevention, 1600 Clifton Rd. NE, Mailstop E02, Atlanta, GA 30333.
CDC also recommends that isolates from certain infections be submitted to the Neisseria Reference Laboratory at CDC for confirmation: John Papp, Ph.D. [email protected]; 404-639-3785, Neisseria Reference Laboratory, Centers for Disease Control and Prevention, 1600 Clifton Rd. NE, Mailstop A12, Atlanta, GA 30333.
These infections comprise those that do not respond to CDC-recommended therapy. See pg. 6, Recommended Testing and Confirmatory Testing for a complete list.
Trends and Treatment
In 1993, ciprofloxacin, a fluoroquinolone, and cephalosporins ceftriaxone and cefixime were the recommended treatments for gonorrhea.
However, in the late 1990s and early 2000s, ciprofloxacin resistance was detected in Hawaii and the West Coast, and by 2004 ciprofloxacin resistance was detected among men who have sex with men (MSM) with gonorrhea.
By 2006, 13.8% of isolates exhibited resistance to ciprofloxacin, and ciprofloxacin resistance was present in all regions of the country, and in the heterosexual population.
On April 13, 2007, CDC stopped recommending fluoroquinolones as empiric treatment for gonococcal infections for all people in the United States. The cephalosporins, either cefixime or ceftriaxone, were the only remaining recommended treatments.
Similar to trends observed elsewhere in the world, CDC has observed recent worrisome trends of decreasing cephalosporin susceptibility, especially to the oral cephalosporin cefixime.
To preserve cephalosporins for as long as possible, CDC has since then made the following changes to its STD Treatment Guidelines:
• In 2010, CDC changed its treatment recommendations to recommend dual therapy for the treatment of gonorrhea and increased the recommended dose of ceftriaxone to 250 mg.
• Following continued declines in cefixime susceptibility, CDC updated its recommendations in 2012 to recommend ceftriaxone plus either azithromycin or doxycycline as the only first-line treatment.
• CDC’s 2015 STD Treatment Guidelines now recommend only one regimen of dual therapy for the treatment of gonorrhea—the injectable cephalosporin ceftriaxone, plus oral azithromycin. Dual therapy is recommended to address the potential emergence of gonococcal cephalosporin resistance.
In 2012 and 2013, there were dramatic decreases in resistance to cefixime. However, resistance levels increased in 2014 for cefixime and azithromycin .
While cefixime is no longer recommended, azithromycin is recommended as part of dual therapy and is also the backbone of every alternative treatment option. CDC has not received any reports of verified clinical treatment failures to any cephalosporin in the United States.
A major challenge to monitoring emerging antimicrobial resistance of N. gonorrhoeae is the substantial decline in the use of gonorrhea culture by many clinicians, as well as the reduced capability of many laboratories to perform gonorrhea culture techniques required for antibiotic susceptibility testing.
Culture testing is when the bacteria is first grown on a nutrient plate and is then exposed to known amounts of an antibiotic to determine the bacteria’s susceptibility to the antibiotic.
The decline in culture testing results from an increased use of newer nonculture-based laboratory technology, such as a diagnostic test called the Nucleic Acid Amplification Test (NAAT).
Currently, there is no well-studied reliable technology that allows for antibiotic susceptibility testing from nonculture specimens. Increased laboratory culture capacity is needed.
CDC recommends that all state and local health department labs maintain or develop the capacity to perform gonorrhea culture, or form partnerships with experienced laboratories that can perform this type of testing.